October self assignment
The most common cause of Ascites is
Cirrhosis of liver
risk factors in this patient :
1. Chronic alcoholism since 40 years
2. Truncal obesity leading to metabolic syndrome causing NAFLD leading to cirrhosis
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6092576/
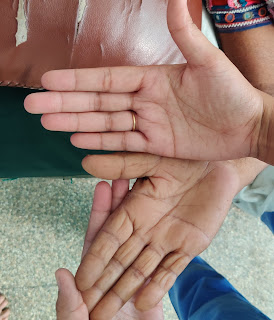
Q2 Bilateral pedal oedema which is of pitting type is due to decrease in the albumin level trends due to course of the disease and long standing cirrhosis causing decrease in the production of proteins causing decrease in the oncotic pressure leading to accumulation of fluid.
as per the given clinical data due to chronic liver disease there was increasing trend of INR which was as high as 4.7 causing bleeding manifestations ( bleeding gums, hematoma formation ) ulcerations are due his limited self practising manoeuvres done in inappropriate conditions such as improper dressing of the wound, not maintaining aseptic conditions , indescriminate use of steroids (self medication) causing ? immune suppression leading to secondary infections hence cellulitis and non healing of wound.
Q3 Reason for Asterexis and constructional apraxia :
Asterixis is a clinical sign that describes the inability to maintain sustained posture with subsequent brief, shock-like, involuntary movements. This motor disorder is myoclonus characterized by muscular inhibition (whereas muscle contractions produce positive myoclonus).[1] Initially described in 1949 by James Foley and Raymond Adams to describe the flapping tremor they observed in liver disease,[2] this clinical sign is not pathognomonic for any condition. However, it may indicate a serious underlying disease process.
https://www.ncbi.nlm.nih.gov/books/NBK535445/
In hepatic encephalopathy (due to cirrhosis of liver ) damage occurs to brain cells due to the impaired metabolism of ammonia is predominantly related to the development of asterixis in hepatic encephalopathy,
pathophysiology of HE
1 role of neurotoxins
2.impaired neurotransmission due to metabolic changes in liver failure, changes in brain energy metabolism, systemic inflammatory response and alterations of the blood brain barrier which produces a wide spectrum of nonspecific neurological and psychiatric manifestations.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5421503/
Gave :
lactulose and rifaximin
mechanism of Giving lactulose :
The human small intestinal mucosa does not have the enzymes to split lactulose, and hence lactulose reaches the large bowel unchanged.
basically three mechanisms have been described on usage of lactulose .
1.First, the colonic metabolism of sugars causes a laxative effect via an increase in intraluminal gas formation and osmolality which leads to a reduction in transit time and intraluminal pH. This laxative effect is also beneficial for constipation.
2. lactulose promotes increased uptake of ammonia by colonic bacteria which utilize the trapped colonic ammonia as a nitrogen source for protein synthesis. The reduction of intestinal pH facilitates this process, which favors the conversion of ammonia (NH3) produced by the gut bacteria, to ammonium (NH4+),[8][9][10] an ionized form of the molecule, unable to cross biological membranes.
3. lactulose also causes a reduction in intestinal production of ammonia. The acidic pH destroys urease-producing bacteria involved in the production of ammonia. The unabsorbed disaccharide also inhibits intestinal glutaminase activity, which blocks the intestinal uptake of glutamine, and its metabolism.
Q4 efficacy of treatment intervention given
high protein diet (2eggs / day) for decreased albumin synthesis
1. Air or water bed to prevent pressure bed sores in the dependent areas
2. Fluid restriction <1.5litres/day so as to decrease of fluid dissemination into the extra vascular space
Salt restriction <2.4gms/day to prevent retention of water due to osmotic gradient as sodium causes retention
3. Inj augmentin 1.2gm IV/BD to prevent secondary bacterial infections
4. Inj pan 40 mg IV/OD
5. Inj zofer 4mg IV/BD
6. Tab lasilactone (20/50)mg BD ( combination of furosemide and aldactone to decrease pedal oedema
If SBP <90mmhg - to avoid excessive loss of fluid
7. Inj vit k 10mg IM/ STAT ( as vitamin K causes coagulation to further prevent bleeding manifestions
8. Syp lactulose 15ml/PO/BD for hepatic encephalopathy
9. Tab udiliv 300mg/PO/BD contain Ursodeoxycholic acid as an active ingredient. It is used to dissolve gall stones in various liver-related disorders such as cirrhosis
10.syp hepameiz 15 ml/PO/OD
11.IVF 1 NS slowly at 30ml/hr to maintain hydration
12. Inj thiamine 100mg in 100mlNS /IV/TID as thiamine deficiency's occur in chronic alcoholics
13.strict BP/PR/TEMP/Spo2 CHARTING HOURLY
14.strict I/O charting
15.GRBS 6th hourly
16.protein x powder in glass of milk TID for protein supplementation and muscle wasting which commonly occurs in cirrhosis patients
17. 2FFP and 1PRBC transfusion to support coagulation pathways
18 .ASD DONE for wound infections and ulcer
CASE 2
Q1 May be ATT were stopped because of his concomitant Chronic liver disease secondary to ? chronic alcoholism as, the ATT first line drugs such as isoniazid and rifampicin are hepatic toxic
LFT is deranged
TB raised
ALP raised
history of watery diarrhoea since 20 days might be due to ?GI infection or
?Rifampicin induced (pseudomembranous colitis) was noticed.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3363060/
Usage of ATT induced hepatotoxicity increased 14-fold in patients with chronic liver diseases (CLD) and liver cirrhosis, more so in those with decompensated disease, probably due to the cirrhosis-associated immune dysfunction syndrome, and case-fatality rates are high.
If hepatotoxicity develops in those with liver cirrhosis, particularly decompensated cirrhosis, the risk of severe liver failure is markedly increased.
Currently, there are no established guidelines for anti-tuberculosis therapy (ATT) in CLD and liver cirrhosis although the need for such guidelines is self-evident.
1. It is proposed that ATT should include no more than 2 hepatotoxic drugs (RIF and INH) in patients with CLD or liver cirrhosis and stable liver function [Child-Turcotte-Pugh (CTP) ≤7],
2. only a single hepatotoxic drug (RIF or INH) in those with advanced liver dysfunction (CTP 8–10) and
3. no hepatotoxic drugs with very advanced liver dysfunction (CTP ≥11).
PZA is contraindicated in the presence of liver disease although some authors believe that PZA is well tolerated in these patients.65–69 Current recommended dose of 15–30 mg/kg has significantly less risk of hepatotoxicity. The frequency of hepatotoxicity in patients who received PZA in doses of 25–35 mg/kg along with RIF and INH was found to be similar to those who received only RIF and INH.
Treatment regimens of anti-tuberculosis therapy in patient with chronic liver disease.21
A. Regimens with only two potentially hepatotoxic drug:
(i) Regimens without INH
(ii) Regimens without PZA
B. Regimens with only one potentially hepatotoxic drug.
C. Regimens with no potentially hepatotoxic drugs.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3940527/
Q2. Bilateral Infiltrations of lung fields noted in CXR PA view
consolidations
?cavitiy in right lung.
Q3. Chronic decompensated liver disease leading to ?portal hypertension
as the tap was transudative based on Lights criteria
although serum albumin was low
Q4.Inj Human Actrapid Insulin s/c 8am - 2pm - 8pm for diabetic management
Inj PAN 40 mg IV/OD
Inj optineuron 1 amp in 100 ml NS Iv/bd for nutritional supplementation such as Vit B12
ATT to be with held for hepatoxicity although should be used based on CPT score mentioned above
Syp lactulose 15ml HS to prevent hepatic encephalopathy
Protein powder 3 to 4 scoops in 1 glass of milk or water QID for protein supplementation
Stop all OHA s
Grbs charting 6th hrly
Strict I/0 charting
High protein diet 4eggs daily for protein supplementation
ORS sachets in 1 litre of water to compensate electrolytes lost due to diarrhoea
Bp charting hourly
Inj PIPTAZ 4.5gm/IV/bd stat - - --> TID
Vit k 10 mg Iv OD for 5 days to prevent forthcoming ?bleeding manifestations
Temp BP PR monitoring 4th hourly
IVF - 1 DNS @50ml/hr for hydration
Nebulisation with salbutamol and mucomist 12th hourly. for ?cough
Inj thiamine 100 mg in 100 ml NS IV TID. for chronic alcoholism.
CASE 3
1. As per the available clinical data nephrotic syndrome have been established
1.Initial management should focus on investigating the cause,
Primary ( idiopathic )
Secondary glomerular pathology
Primary causes include
FSGS
membranous glomerular nephropathy
minimal change
MPGN
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2394708/
Secondary causes of nephrotic syndrome
Other diseases
* Diabetes mellitus
* Systemic lupus erythematosus
* Amyloidosis
Cancer
* Myeloma and lymphoma
Drugs
* Gold
* Antimicrobial agents
* Non-steroidal anti-inflammatory drugs
Infections
* HIV
* Hepatitis B and C
* Mycoplasma
* Syphilis
* Malaria
* Schistosomiasis
* Filariasis
* Toxoplasmosis
Congenital causes
* Alport’s syndrome
* Congenital nephrotic syndrome of the Finnish type
* Pierson’s syndrome
* Nail-patella syndrome
* Denys-Drash
2. Identifying complications such as
thromboembolism
Infections
hyperlipidemia
acute renal failure
3. Managing the symptoms of the disease such as protein loss, pedal oedema,
and hyper coagulable state which still did not manifested in this patient or need not be in many
cases.
A renal biopsy would be helpful in establishing the cause of which type of glomerular pathology is causing the nephrotic syndrome. however if the nephrotic syndrome is secondary to other above mentioned cases ruling out that gives a better picture rather than going straight away for biopsy ..
PROS of renal biopsy : Gives a specific diagnosis, reflect the disease activity, provide information to allow decisions and planned treatment..It remains a valuable clinical tool and of particular benefit when other investigations fail to diagnose.
CONS: Dull ache pain around the needle entry site... Sometimes perirenal haematoma forms leading to severe loin pain...The mean decrease in Hb after biopsy is approximately 1g/dl...Visible hematuria in 3.5% ,Need for blood transfusion in 0.9% and need for intervention to control bleeding in 0.7% and Death in 0.02 %....Rare complications include infection, damage to blood vessels or other organs or urine leak... Sometimes development of arteriovenous fistula.


Comments
Post a Comment