35 year old with pain abdomen
CHIEF COMPLAINTS :
35 year old female who is a wig maker survived with 3 kids resident of nakrekal came to casuality with complaints of pain abdomen since Friday & vomiting’s since Friday, dyspepsia since 10 days
HOPI & PAST HISTORY :
Married at the age of 17 years , non consanguineous.
1st child at 18 years - death of the first child at 24years due to varicella zoster.
2nd child at age of 21 years - gave birth to female child , now married
3rd child at the age of 23 years -gave birth to female child , now married
4th child at the age of 24years - gave birth to male child currently 10th class .
HOPI & PAST H/O:
Patient was apparently asymptomatic 7 years back met with an RTA ,auto vs lorry sustained injury to her head , no loss of consciousness, no history of headache , no history of vomitings , was incidentally diagnosed with type -2 DM on irregular medication since then.
DAILY ROUTINE :
Wakes up at 5:30 am in the morning , gets ready for work and goes for work and comes back by 11:00 am and does house hold work , and sits at a kirana shop or play with her grand daughter .
Earns around 4000/- month approx .
Now, presenting with complaints of pain abdomen diffuse in type ,squeezing type of pain , associated with vomitings 2-3 episodes non bilious , non projectile , non foul smelling , non blood tinged .
Didn’t pass flatus since 2 days
Passing stools small amount.
History of bloating , belching since 5 years using antacids .
Passage of hard stools since 2 months ( Bristol stool chart - type 1 )
At presentation:
Patient is consicous , coherent and Co-operative
Febrile to touch 99.1 F
Bp: 110/80mmhg
Pulse :119 bpm regular normal volume
CVS : s1 s2 no murmur
Rs : fine crepts in left infra axillary and infra scapular area
CNS : HMF intact
Spo2: 92% RA
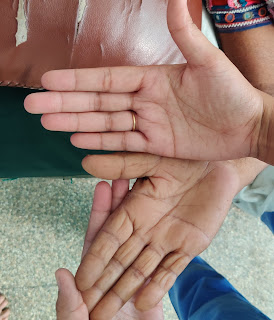
Pallor + Icterus - , cyanosis - , clubbing - , lymphadenopathy - , pedal Edema +
Personal history : mixed diet, appetite reduced
Regukar bowel and bladder movements
NON SMOKER AND NON ALCOHOLIC
Family history : mother is hypertensive, expired due to cva after bedridden for 6 months .
Drug history : NONE









Comments
Post a Comment